Looks like they were doing that gas dispersal test at Westminster station this morning
All posts by alex
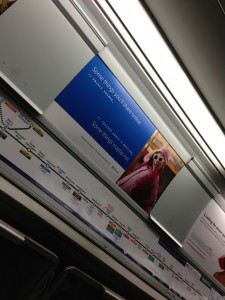
“Your privacy is our priority”. Bit…
“Your privacy is our priority”. Bit of an unfortunate tube advert there Microsoft. #prism
Worst email ever (and I have no idea…
Erm…
Ducklings! #se16
Ducklings! #se16
This is like US immigration asking if…
I just did SCIENCE with @Polypompholyx
Show me the data
I was published in the BMJ today, having been asked to write an expanded version of this blog post.
The patient Alex Lomas is taking a biological drug for Crohn’s disease, and he wants to know why the maker is trying to prevent disclosure of trial data that may well affect him
I have an obsession with data. I have instruments in my house so I know how hot each room is and to warn me if the fridge door has been open for too long. I record my weight and blood pressure using devices connected to the internet so that I can monitor long term trends. I use my smartphone to track how much walking and exercise I do.
I was diagnosed with Crohn’s disease about 20 years ago, when awareness of inflammatory bowel diseases was not as high as it is today.1 The treatment decisions made at the time of my diagnosis had unfortunate side effects for me as a teenager. High doses of prednisolone led to Cushing’s syndrome, and I was mercilessly teased about my appearance at school. With time came a reduction in the dose of steroids required, but I had to take them throughout my 20s, and control of my symptoms was still inadequate.
As a patient with Crohn’s disease, I take an active interest in my day-to-day health, but I also routinely scan news media and journal sites for new treatments and for changes to current best practice in the management of my condition. I often arrive at appointments with my consultant armed with PDFs printed from the BMJ, the Cochrane Collaboration, and the National Institute for Health and Care Excellence (NICE) to discuss the latest trials and treatment options. Yes, I’m afraid I’m one of those patients.
Three years ago my consultant suggested a new course of treatment with adalimumab (Humira), an anti-TNFα monoclonal antibody. My local primary care trust approved this new drug, which costs £352 per injection, and which I administer myself by injection each fortnight.2 Since I started taking adalimumab I have the least symptoms since diagnosis. I am no longer taking steroids; I have started to recover from 15 years of side effects; and I spend less time in clinical care and off work on sick leave.
However, anecdotes are not the foundation of evidence based medicine, and nor are they a rational basis for evaluating the cost of a treatment. On 1 April 2013 responsibility for commissioning transferred from my primary care trust to the local clinical commissioning group, bringing into sharp focus the question of whether the NHS is getting value for money in continuing my treatment.
Equally importantly, I want to be able to evaluate the benefits and risks of these costly pharmaceuticals with which I inject myself regularly. Biologicals are relatively new, and have failed spectacularly in clinical trials.3 Who knows what 20 or 30 years of data from clinical use might bring? The most recent Cochrane review of biologicals looked at nine studies, and, although it found that they were effective, it noted that none of the trials allowed for an assessment of long term adverse events nor had any trials been undertaken that compared efficacy among the available biologicals.4 My consultant recently told me that no trials had been done to determine what the minimum effective dose of adalimumab was, nor would there likely ever be; a drug company has no interest in showing you can take less of something.
Part of NICE’s approval for the use of adalimumab in treating Crohn’s disease was the recommendation that a register of patients being treated with biologicals be set up to track long term outcomes and relapse rates after withdrawal of treatment, something patient groups welcomed.5 Unfortunately it seems that such registers are fragmented, with registers of patients with rheumatoid arthritis held independently from registers of patients with inflammatory bowel disease, or are still at pilot stage.6
As a patient, I need clinicians to interpret trial data and systematic reviews of new and existing treatments so we can come to appropriate decisions about my treatment, but what if even experts don’t get to see the whole picture? How can we even know what trials are being run?
I was therefore dismayed to learn that Abbvie, the maker of adalimumab, are seeking a legal injunction to prevent the European Medicines Agency from disclosing trial data submitted during the drug’s approval process.7 With such a new drug, it is vital that all data, whether it’s good news or bad, are made available so that I, my consultant, and the care commissioning group can make informed decisions about the efficacy and cost effectiveness of treatments.
As the drug industry and medical profession as a whole move towards the registration of all trials, and the publication of all trial data—in no small way thanks to the All Trials initiative (www.alltrials.net)—this decision by Abbvie is a backwards step and is offensive to trial participants, patients, and the wider public who ultimately pick up the tab.
Notes
Cite this as: BMJ 2013;346:f2336
Footnotes
-
Competing interests: I have read and understood the BMJ Group policy on declaration of interests and have no relevant interests to declare.
-
Provenance and peer review: Not commissioned; not externally peer reviewed.
References
- ↵
- ↵
Adalimumab. British National Formulary. www.medicinescomplete.com/mc/bnf/current/PHP6632-humira.htm.
- ↵
Goodyear M. Learning from the TGN1412 trial. BMJ 2006;0:38797.635012.47
- ↵
- ↵
NACC. A good decision from NICE on antiTNF treatments for Crohn’s disease. 2010. www.nacc.org.uk/downloads/media/NACC_statement_antiTNFs_4_March_2010.pdf.
- ↵
Alrubaiy L, Williams J, Morgan J. P422. The Biologics Register for inflammatory bowel disease in the UK: setting the clinical dataset and the IT infrastructure. ECCO, 2013. https://www.ecco-ibd.eu/publications/congress-abstract-s/item/p422-the-bi.html.
- ↵
Oxford
We went to Oxford a couple of nights. It was cold. We stayed in a prison.